Cardiac transplantation is a widely accepted therapy for the treatment of end-stage congestive heart failure. Most candidates for cardiac transplantation have not been helped by conventional medical therapy and are excluded from other surgical options because of the poor condition of the heart. About 45% of the candidates have ischemic cardiomyopathy; however, this percentage is rising because of the increase in coronary artery disease in younger age groups. Of the candidates, 54% have some form of dilated cardiomyopathy, which often has an unclear origin. The remaining 1% of candidates fall into the category of other diseases, including congenital heart disease, that are not amenable to surgical correction.
Candidacy determination and evaluation are key components of the process, as is postoperative follow-up care and immunosuppression management. Proper execution of these steps can culminate in an extremely satisfying outcome for both the physician and patient.
Christian Barnard performed the first successful heart transplant in a human in 1967 in South Africa. The origins of the procedure date to 1905, when Alexis Carrel transplanted a puppy's heart into the neck of a dog. Because of the lack of immunosuppression, the experiment was unsuccessful; however, the work spurred numerous investigations that culminated in the success the procedure has today. Early investigators included Frank C. Mann of the Mayo Clinic, V.P. Demikov of the Soviet Union, and Marcus Wong. These early efforts in transplantation were thwarted by the infancy of cardiopulmonary bypass and a lack of understanding of the immune system. As knowledge in these areas advanced, so did the field of cardiac transplantation.
The clinical use of cyclosporine as an immunosuppressant revolutionized the field of cardiac transplantation in 1983. Recipient survival rates improved, thus producing an explosive increase in the number of transplant centers offering cardiac transplantation. The remaining limiting factor was the number of available organ donors.
During the cardiac transplantation procedure, the ventricles are excised, leaving the great vessels, right atrium, and left atrium of the recipient.
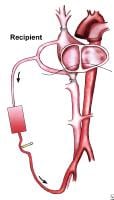 View of the recipient's chest after the heart is removed, with the patient on cardiopulmonary bypass.
View of the recipient's chest after the heart is removed, with the patient on cardiopulmonary bypass.The donor heart is then sewn to these areas.
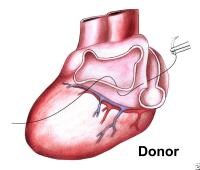 Suturing of the donor heart. Note that the left atrial anastomosis is performed first.
Suturing of the donor heart. Note that the left atrial anastomosis is performed first.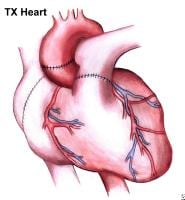 The completed operation. Note the suture lines on the now-implanted heart.
The completed operation. Note the suture lines on the now-implanted heart.A recent trend has been to revert to bicaval anastomoses rather than right atrial anastomoses in an attempt to decrease the incidence of postoperative tricuspid insufficiency.
In the transplantation process, the sinoatrial nodes of the donor and recipient remain intact, and both are present within the recipient. For approximately 3 weeks after surgery, the electrocardiogram demonstrates 2 P waves; however, the heart rate and electrical activity of the new heart are purely dependent on the intrinsic electrical system of the heart and not on the neurological input from the recipient.
Indications
The general indications for cardiac transplantation include deteriorating cardiac function and having a prognosis of less than 1 year to live.
Specific indications
- Dilated cardiomyopathy
- Ischemic cardiomyopathy
- Congenital heart disease for which no conventional therapy exists or that conventional therapy has failed
- Ejection fraction less than 20%
- Intractable angina or malignant cardiac arrhythmias for which conventional therapy has been exhausted
- Pulmonary vascular resistance of less than 2 Wood units
- Age younger than 65 years
- Ability to comply with medical follow-up care
No comments:
Post a Comment